Sexual Health After Prostate Surgery
Sexual health is a vital aspect of overall well-being for men, regardless of age. For those who undergo prostate surgery — particularly radical prostatectomy, which involves the surgical removal of the prostate gland often due to prostate cancer — sexual health can become a complex and sensitive issue. In the United States, prostate cancer is the second most common cancer among men, with nearly one in eight men diagnosed during their lifetime.
Even with advances in surgical techniques, many men encounter sexual side effects after surgery, such as erectile dysfunction, changes in libido, and alterations in orgasmic function. These side effects are not exclusive to older individuals. Increasing awareness and early screening mean that younger men are also facing these issues and should be equally informed. Men in their 30s to 50s are experiencing early diagnoses and are beginning to consider long-term sexual recovery measures earlier in life.
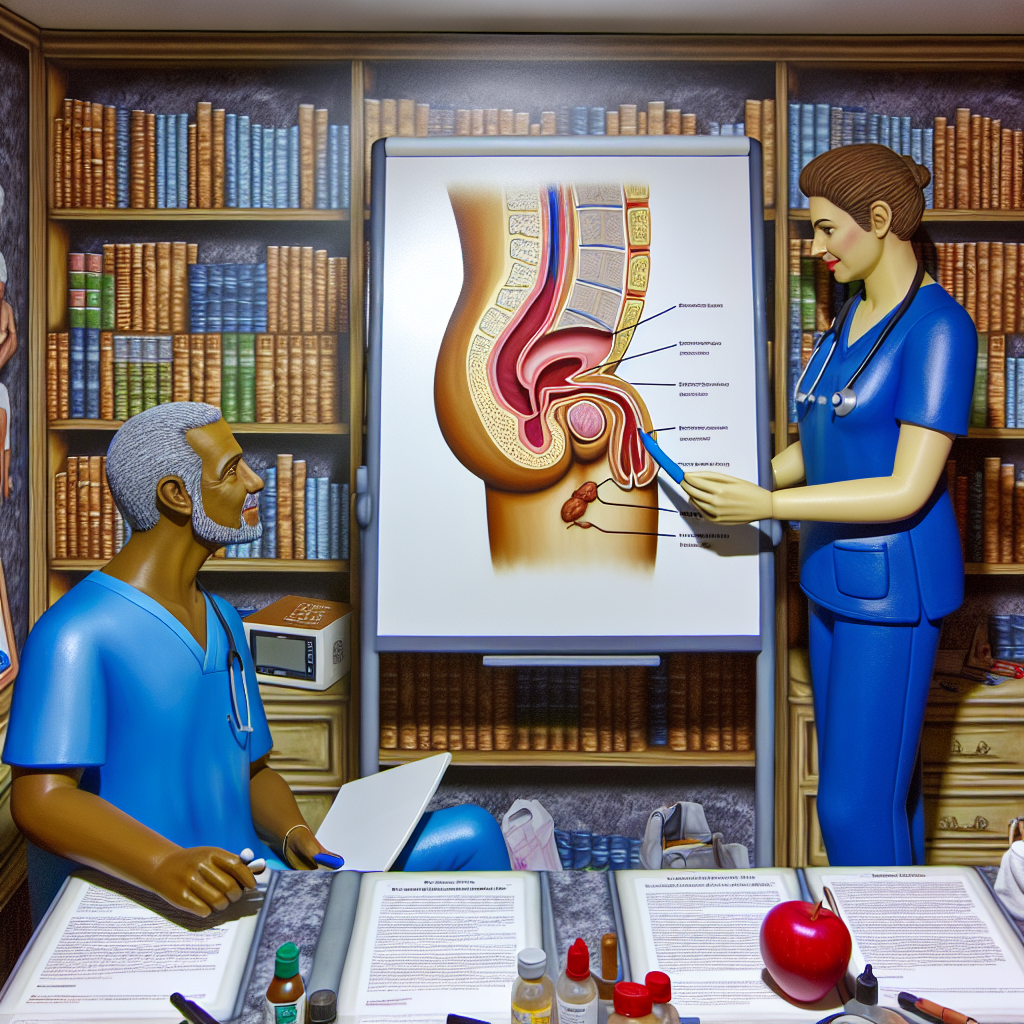
The root cause of these side effects lies in the prostate’s location, which is close to the nerves and blood vessels responsible for erection. Even with nerve-sparing prostatectomy techniques, minor nerve damage may occur. The removal of the prostate and seminal vesicles also results in dry orgasms, where ejaculation no longer occurs. This alteration can be jarring and psychologically unsettling for many, especially if unanticipated.
Fortunately, with time and intervention, sexual function can often return or dramatically improve. Recovery strategies include oral medications, penile rehabilitation protocols, vacuum erection devices (VEDs), and, for more persistent cases, penile implants. All treatments are most effective when begun soon after surgery. Equally important is addressing emotional and mental changes; depression, anxiety, and relationship stress are common and manageable with the right support.
This article explores scientific advancements, proven medical practices, and emotional support resources that empower men to regain a fulfilling sex life following prostate surgery — offering insight and support for men at every stage of adulthood.
Medical Studies & Features
Over the last two decades, extensive research has targeted improved sexual functioning post-prostatectomy. A critical turning point was the development of the nerve-sparing prostatectomy by Dr. Patrick Walsh in the 1980s. This technique focuses on preserving the delicate nerve bundles essential for a man’s ability to achieve erections.
A 2011 study published in JAMA (Journal of the American Medical Association) followed over 1,200 men post-surgery. It found that while 60% experienced erectile dysfunction immediately, many regained function within one to two years, especially those who had undergone nerve-sparing surgery. Important predictors of successful sexual recovery included younger age, strong pre-surgery erectile function, and surgeon experience, highlighting the importance of patient education and informed decision-making during surgeon selection.
Penile rehabilitation is a proactive approach to restoring function. The American Urological Association (AUA) recommends early use of PDE5 inhibitors like sildenafil (Viagra) and tadalafil (Cialis). These medications promote blood flow to erectile tissue, minimizing long-term damage. They are most effective when initiated within several weeks after surgery and used consistently, often in combination with vacuum erection devices or direct penile stimulation. Success depends on patient commitment and regular follow-through with rehabilitation protocols.
A promising innovation is low-intensity shockwave therapy (LiSWT), a non-invasive treatment aimed at enhancing penile blood flow and revitalizing nerve function. While not yet considered mainstream, a 2020 review in the British Journal of Urology International reported highly encouraging preliminary outcomes, suggesting this may become a future cornerstone for post-operative sexual recovery.
In addition to physical concerns, strong links have been identified between sexual dysfunction and mental health. The Prostate Cancer Foundation notes high rates of depression and anxiety in patients post-surgery. The emotional toll can be as debilitating as the physical changes. Understanding these challenges and seeking therapy, couples counseling, or support groups can guide men toward emotional recovery. Healthcare providers are increasingly recommending integrated care that treats both body and mind.
Beyond erections, issues like climacturia (urine leakage during orgasm) and less intense orgasms also affect quality of life. Though distressing, these symptoms are treatable. Pelvic floor exercises, or Kegel exercises, have demonstrated value in improving urinary control and enhancing overall sexual satisfaction. A 2019 study in European Urology found that structured pelvic floor therapy led to a 30% improvement in climacturia symptoms compared to control groups. Physical therapists specializing in pelvic health can play a vital role in guiding these techniques.
Conclusion
Sexual health after prostate surgery presents challenges, but is far from a dead-end. Advances in surgical methods, proactive treatment plans, and psychological care contribute to positive outcomes for most men. Restoring intimacy, pleasure, and confidence depends on early intervention, education, and clear communication with healthcare providers and loved ones.
Recovery is a multifaceted process — not just physical, but emotional and psychological. Men of any age — including those diagnosed young and those maintaining relationships later in life — can reclaim their sexual well-being. Awareness and action are key. Embracing available treatments and support systems empowers men to navigate recovery with hope and confidence.
Concise Summary
Sexual function after prostate surgery often declines due to nerve and tissue disruption; however, recovery is possible with early treatment and support. Techniques like nerve-sparing surgery, penile rehabilitation with medications, vacuum devices, pelvic floor therapy, and psychological counseling greatly enhance outcomes. New methods such as shockwave therapy are also emerging. Emotional health and open partner communication are just as critical as medical therapies. With a multifaceted approach, men can regain sexual confidence and pleasure post-prostatectomy.
References
- JAMA: Quality of Life and Satisfaction with Outcome among Prostate Cancer Survivors
- European Urology: Efficacy of Pelvic Floor Muscle Training
- BJUI: Shock Wave Therapy for ED After Prostatectomy
- AUA Guidelines: Early Penile Rehabilitation
- Prostate Cancer Foundation: Dealing with Emotional Impact

Dominic E. is a passionate filmmaker navigating the exciting intersection of art and science. By day, he delves into the complexities of the human body as a full-time medical writer, meticulously translating intricate medical concepts into accessible and engaging narratives. By night, he explores the boundless realm of cinematic storytelling, crafting narratives that evoke emotion and challenge perspectives. Film Student and Full-time Medical Writer for ContentVendor.com