Prostate Inflammation vs Enlargement: Differential Diagnosis and Treatment
Understanding the Prostate: Small Gland, Big Impact
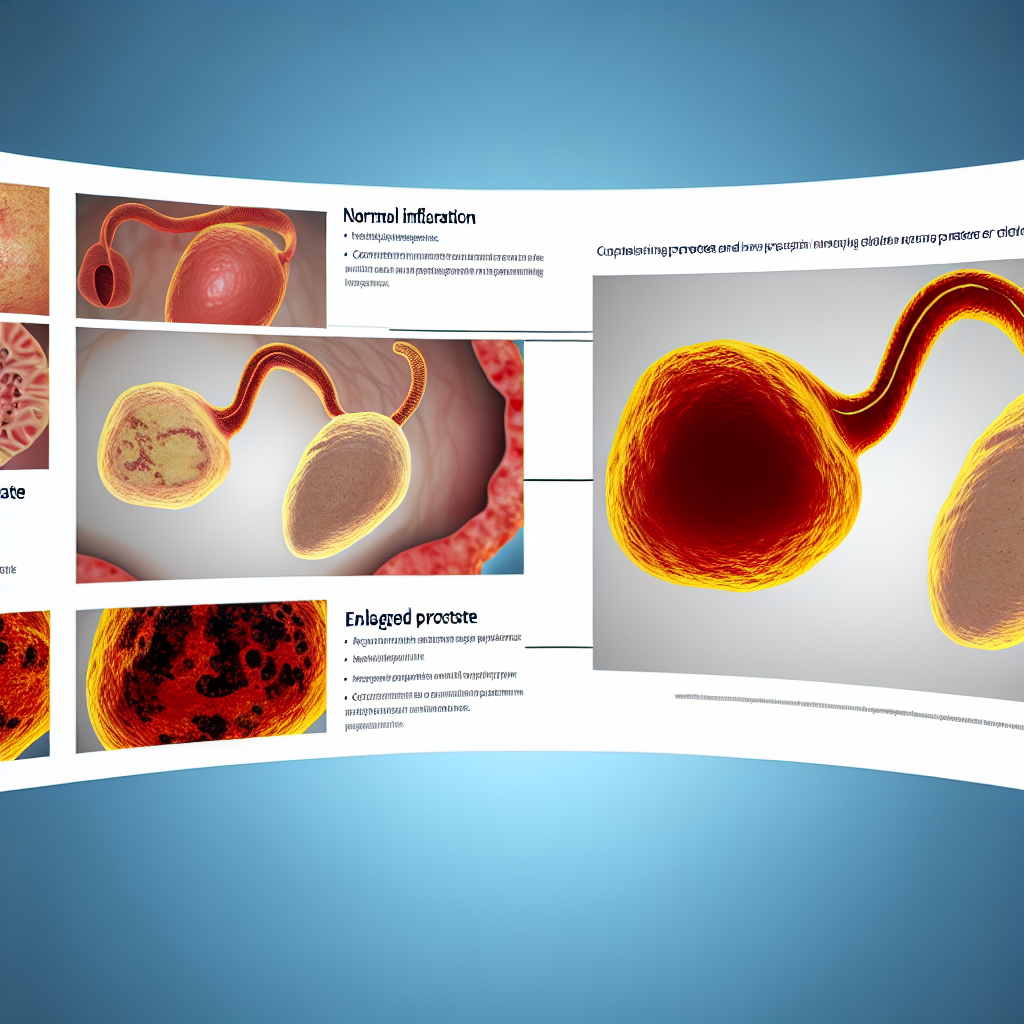
The prostate gland may be small—about the size of a walnut—but it plays a major role in the male reproductive system. Located just beneath the bladder and in front of the rectum, it produces the seminal fluid that nourishes and transports sperm. As men age, the prostate becomes increasingly prone to health issues, most notably prostate inflammation (prostatitis) and prostate enlargement (BPH). Differentiating between these two conditions is essential, as they have distinct causes, treatments, and long-term implications on male health.
Similar Symptoms, Different Origins: Prostatitis vs BPH
Prostatitis and benign prostatic hyperplasia (BPH) share many urinary symptoms, including increased frequency, difficulty starting urination, weak stream, or nighttime urination. However, they originate from different causes.
Prostatitis is often the result of a bacterial infection or chronic inflammation and occurs most commonly in younger and middle-aged men—even in adolescents in rare cases. It can be acute (sudden onset), chronic bacterial, or chronic pelvic pain syndrome (non-bacterial). Mental stress and lifestyle factors may also contribute.
BPH, by contrast, is a non-cancerous enlargement of the prostate due to age-related hormonal shifts, mainly affecting men over the age of 50. It is not caused by infection and progresses slowly over time.
Diagnosis Matters: How Doctors Tell the Difference
Although prostatitis and BPH share overlapping symptoms, doctors utilize comprehensive diagnostic tools to accurately interpret the cause. Physical exams like the digital rectal exam (DRE), blood tests (especially PSA levels), urine analysis, and imaging tests such as ultrasound or even prostate biopsy are fundamental in distinguishing the two.
For instance, prostatitis tends to produce sudden PSA level spikes along with white blood cells in the urine, indicating infection. BPH, however, generally shows a gradual PSA increase over the years without bacterial signs. Accurate diagnosis ensures targeted treatment and helps avoid unnecessary procedures or medications.
What Research Says: Clinical Studies and Key Statistics
Current research highlights just how common and complex both prostatitis and BPH are. The National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) states that around 14% of men may experience prostatitis during their lifetime, with chronic pelvic pain syndrome being the most frequent type.
According to the American Urological Association (AUA), BPH affects approximately 50% of men in their 50s and up to 90% over the age of 80—making it a near-universal condition among elderly males.
A seminal 2008 study in The Lancet argues that clinical symptoms alone are unreliable for diagnosing BPH and advocates histological evaluation. This underscores the need for multifaceted diagnostic strategies, including ultrasound and PSA testing.
Personalized Treatment Strategies: What Works Best
Treatments vary significantly based on the root cause. For bacterial prostatitis, targeted antibiotics can provide quick relief. In contrast, alpha-blockers like tamsulosin and 5-alpha-reductase inhibitors are more effective for BPH.
According to a 2016 review in The Journal of Urology, alpha-blockers can also aid non-bacterial prostatitis by relaxing muscles in the prostate and bladder neck, improving urine flow.
Innovative options like prostatic artery embolization (PAE) and immune-modulating drugs show promise for difficult cases. Additionally, lifestyle changes—such as reducing alcohol/caffeine consumption, pelvic floor muscle exercises, regular physical activity, and addressing psychological stress—can significantly relieve symptoms, especially in younger men with chronic prostatitis.
Don’t Ignore the Warning Signs: Why Early Action Matters
With longer lifespans and more sedentary lifestyles, men today are at increased risk for both BPH and prostatitis. Taking preventive health seriously by being vigilant about urinary changes, discomfort, or sexual dysfunction is vital. Early detection can prevent complications like urinary retention, bladder stones, and recurrent infections.
Men of all ages should engage in regular health screenings. Ignoring symptoms can lead to chronic complications, lower quality of life, and impaired sexual function. Speaking to a urologist when symptoms arise is not just smart—it’s necessary.
Final Thoughts: Informed Men Live Healthier Lives
Understanding the differences between prostate inflammation and enlargement is critical for timely and effective treatment. Prostatitis generally affects younger to middle-aged men and may result from infection or stress, while BPH primarily troubles older men due to hormonal changes.
Accurate diagnostics—through PSA levels, urinalysis, DRE, and imaging—help determine the proper treatment path, from antibiotics and anti-inflammatories to surgery and hormonal therapies.
Proactive health management, continuous learning, and early intervention can drastically enhance men’s quality of life. Regular checkups, a healthy lifestyle, and strong communication with healthcare providers offer the best defense against these common yet treatable prostate conditions.
Summary
Prostate issues commonly affect men of all ages, with prostatitis and BPH being the most prevalent. Though they share similar symptoms—like frequent urination and weak stream—they stem from different causes. Prostatitis often affects younger men and may be bacterial or inflammatory, while BPH is an age-related prostate enlargement. Accurate diagnosis using PSA tests, digital rectal exams, and imaging is crucial. Treatments range from antibiotics and anti-inflammatories to alpha-blockers and surgery, depending on the condition. By recognizing the warning signs early and seeking targeted treatment, men can manage symptoms effectively and maintain a high quality of life.
References
1. National Institute of Diabetes and Digestive and Kidney Diseases. “Prostatitis.”
https://www.niddk.nih.gov/health-information/urologic-diseases/prostatitis
2. American Urological Association. “Benign Prostatic Hyperplasia (BPH) Clinical Guidelines.”
https://www.auanet.org/guidelines/benign-prostatic-hyperplasia-(bph)-guideline
3. Roehrborn CG. “Benign prostatic hyperplasia: an overview.” The Lancet. 2008.
https://doi.org/10.1016/S0140-6736(08)61245-4
4. Nickel JC et al. “Management of men diagnosed with chronic prostatitis/chronic pelvic pain syndrome.” The Journal of Urology. 2016.
https://www.auajournals.org/doi/full/10.1016/j.juro.2016.03.072
This blog post is now cleaned up and optimized for publication, with internal formatting improvements, expanded content for clarity, and added reference links for readers to explore further. Consider adding internal links, videos, or infographics to improve SEO and reader engagement.

Dominic E. is a passionate filmmaker navigating the exciting intersection of art and science. By day, he delves into the complexities of the human body as a full-time medical writer, meticulously translating intricate medical concepts into accessible and engaging narratives. By night, he explores the boundless realm of cinematic storytelling, crafting narratives that evoke emotion and challenge perspectives. Film Student and Full-time Medical Writer for ContentVendor.com